Muckle-Wells Syndrome
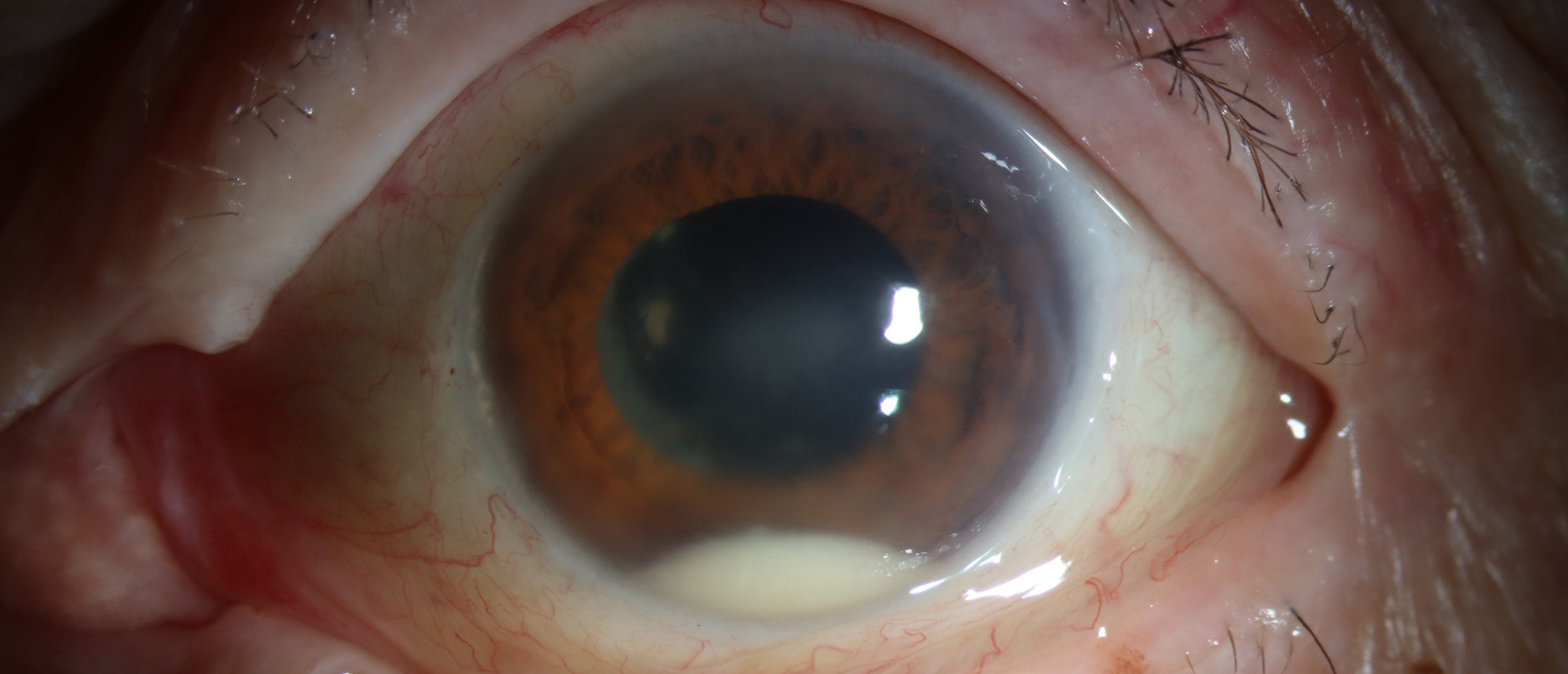
A patient with a past ocular history of retinal vasculitis with subretinal hemorrhage, vitreous hemorrhage, herpetic keratitis, and cataract surgery presented to the emergency room due to sudden onset blurred vision and retrobulbar pain of the left eye. The patient reported low-dose prednisone use for joint pain. On examination, best corrected visual acuity was 20/250 in the right eye and HM in the left eye. Intraocular pressure was 14 and 16. Slit lamp examination was notable for left eye lid edema and erythrma, bilateral central corneal opacities with 3+ guttae, 4+ cell with fibrin and x<1mm layering hypopyon in the left eye, and posterior chamber intraocular lenses of both eyes. Fundus exam of the right eye was notable for pigmentary changes, atrophy, and few hemorrhage. There was no view of the left eye fundus due to diffuse vitreous hemorrhage. B-scan of the left eye was notable for a retinal detachment spanning 1:30 to 9:30 with moderately dense, diffuse and mobile subretinal opacities partially layered inferiorly. Broad uveitic laboratory workup was negative. Upon further history inquiry, the patient had previously been diagnosed with Muckle-Wells Syndrome (a Cryopyrin-Associated Periodic Syndrome). Intense topical steroids, topical cycloplegics, and oral steroids were initiated. Over several weeks the vitreous hemorrhage was found to clear and the retinal detachment was found to be exudative and also started to slowly resolve. Vision remained at HM.
Presentation Date: 12/19/2024
Issue Date: 02/28/2025
Please log in or click on ENROLL ME to access this course.