Leber Hereditary Optic Neuropathy (LHON)
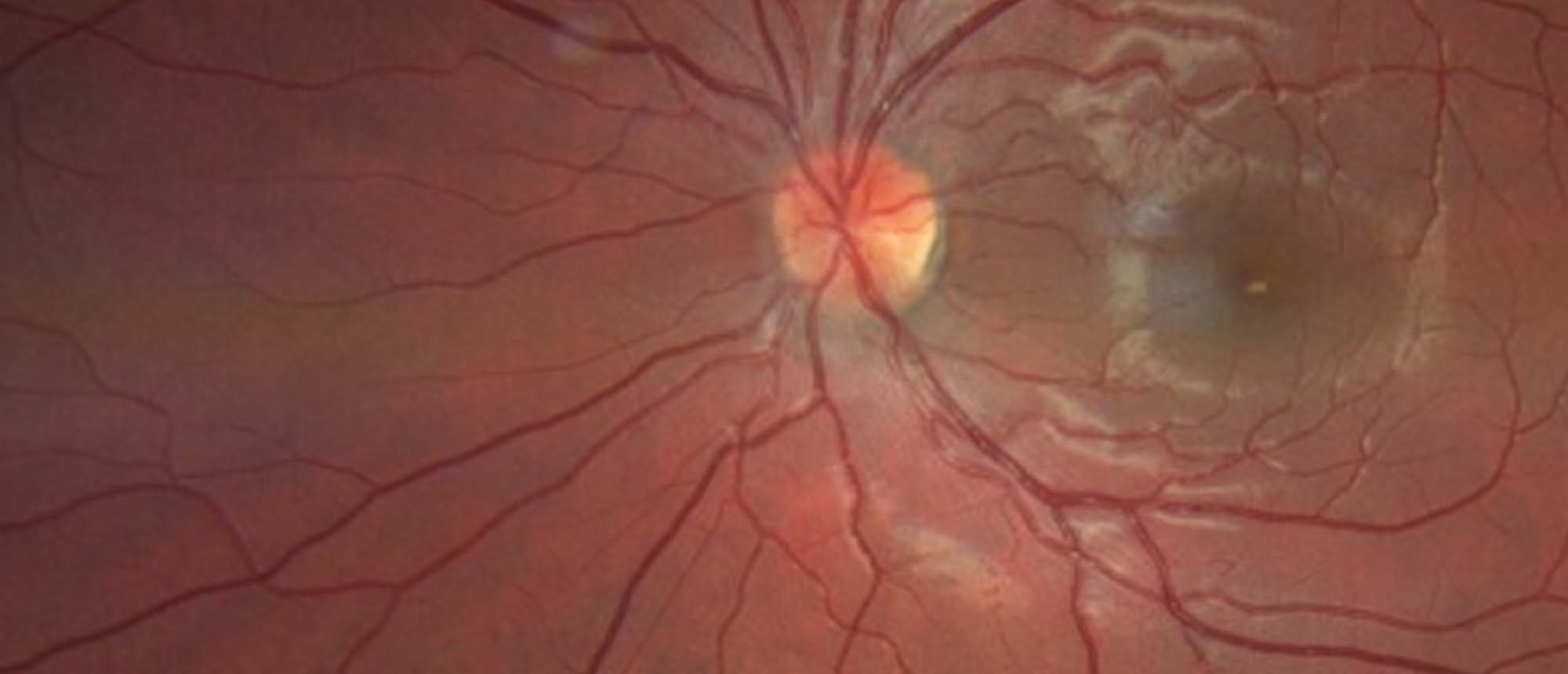
A previously healthy patient presented to the emergency department (ED) with a 2-week history of bilateral blurry vision associated with painful eye movement. The patient denied eye redness, eye discharge, photophobia, double vision, or headache. The ophthalmic exam showed best-corrected visual acuity (BCVA) OD 20/200 OS 20/60, color plates were OD 1/10 OS 3/10, no afferent pupillary defect (APD), and mild optic disc pallor. Humphrey visual field (HVF) showed mildly reduced foveal threshold and retinal nerve fiber layer (RNFL) and ganglion cell layer (GCL) thickness were all normal. Orbital MRI was questionable for bilateral optic and peri-optic neuritis. Full autoimmune, infectious, and inflammatory labs were unremarkable. The patient was given IV methyl-prednisone followed by oral prednisone. BCVA improved to OD 20/150 OS 20/40 and color plates of OD 3/11 OS 7/11. Four months later the patient reported a drop of vision associated with mild ocular pain. The ocular exam showed BCVA OD 20/400 OS 20/150 and temporal optic disc pallor. HVF showed OD cecocentral scotoma with inferonasal defect and OS central scotoma. RNFL and GCL thickness were all reduced. Repeat orbital MRI showed mild intra-orbital enhancement. IV methylprednisolone followed by oral prednisone was started with no improvement. Repeat neuromyelitis optica (NMO) and myelin oligodendrocyte glycoprotein (MOG) antibodies were negative. Full nutritional and toxic lab studies were unremarkable. The patient was started on a 5-day course of plasmapheresis for suspicion of seronegative NMO but with no improvement. Finally, the molecular vision laboratory (MVL) genetic study came out positive for the COX gene which could be associated with Leber hereditary optic neuropathy (LHON). Idebenone 300 mg TID was prescribed.
Presentation Date: 02/17/2022
Issue Date: 03/04/2022
Please log in or click on ENROLL ME to access this course.