Long Anterior Zonules and Pigment Dispersion Syndrome-Variant
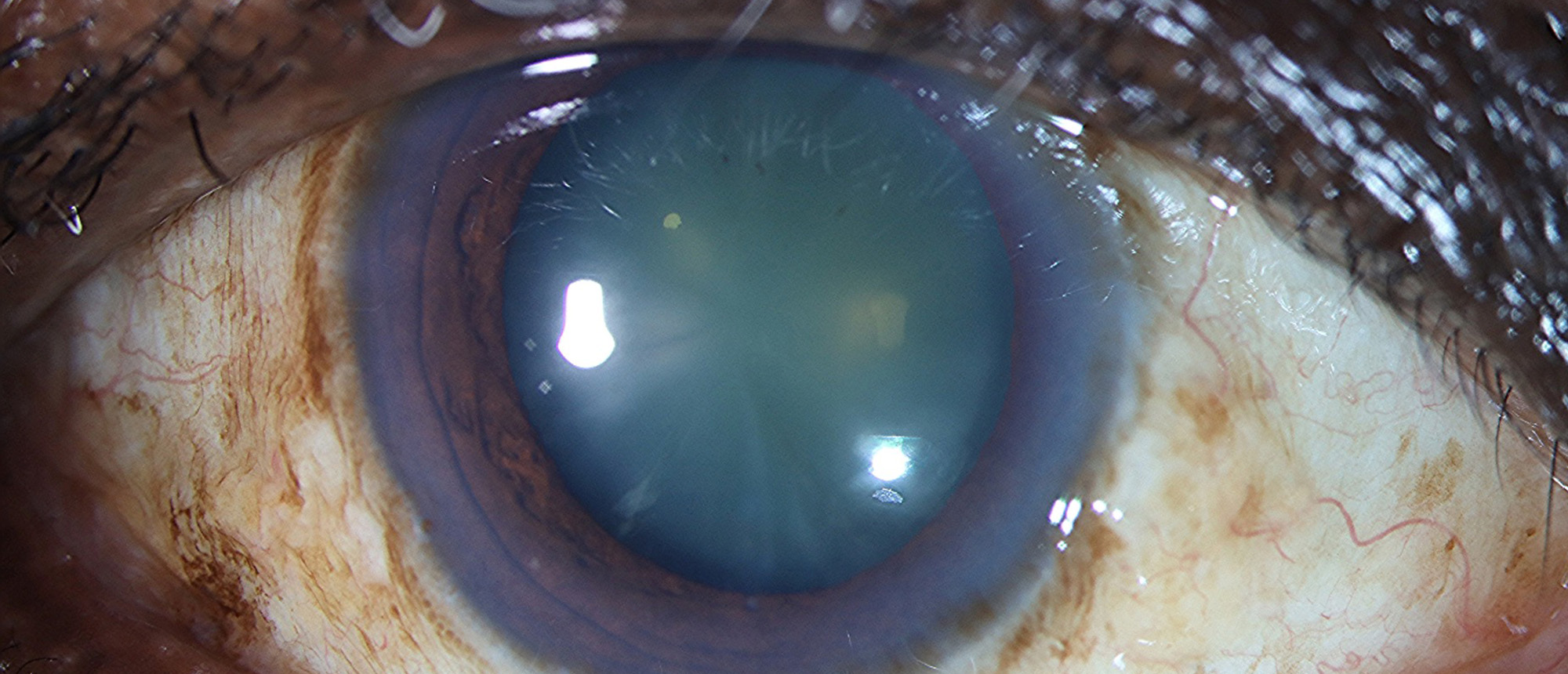
A patient was referred for cataract evaluation with decreased vision in the right eye. The patient had a past ocular history of cataracts of both eyes, corneal scar of the right eye, and intermittent subretinal fluid in the right eye not responsive to intravitreal anti-VEGF agents. Upon presentation, best corrected visual acuity was 20/40 in the right eye, with IOP of 25 mmHg. Gonioscopy revealed angles open to trabecular meshwork 360 in both eyes with heavy pigmentation and inferior Sampaolesi line. Slit lamp examination disclosed a corneal scar in the right eye, nuclear sclerotic cataracts of both eyes, and fine radially oriented pigmented lines on the anterior lens capsule in both eyes. Dilated fundus exam disclosed pigmentary mottling in the macula of both eyes and peripapillary pigmentary changes in the left eye. OCT demonstrated macular PEDs in both eyes without sub-retinal fluid. The anterior capsular findings were favored to represent anomalous long anterior zonular insertion (LAZ) in both eyes, which fit with the patient’s overall clinical picture and demographics. She underwent genetic testing which demonstrated a pathogenic PDE6B mutation for AR Retinitis Pigmentosa, but was otherwise unrevealing. Her Multifocal ERG was normal in both eyes. The patient underwent successful cataract surgery in the right eye which was moderately complex due to her small zonule free zone (ZFZ) and LAZ phenotype. Her anterior capsule was preserved and sent for analysis via scanning electron micrograph. The patient was diagnosed with Long Anterior Zonules (LAZ) and Pigment Dispersion Syndome-Variant in both eyes.
Presentation Date: 05/23/2024
Issue Date: 06/07/2024
Please log in or click on ENROLL ME to access this course.