Idiopathic Intracranial Hypertension
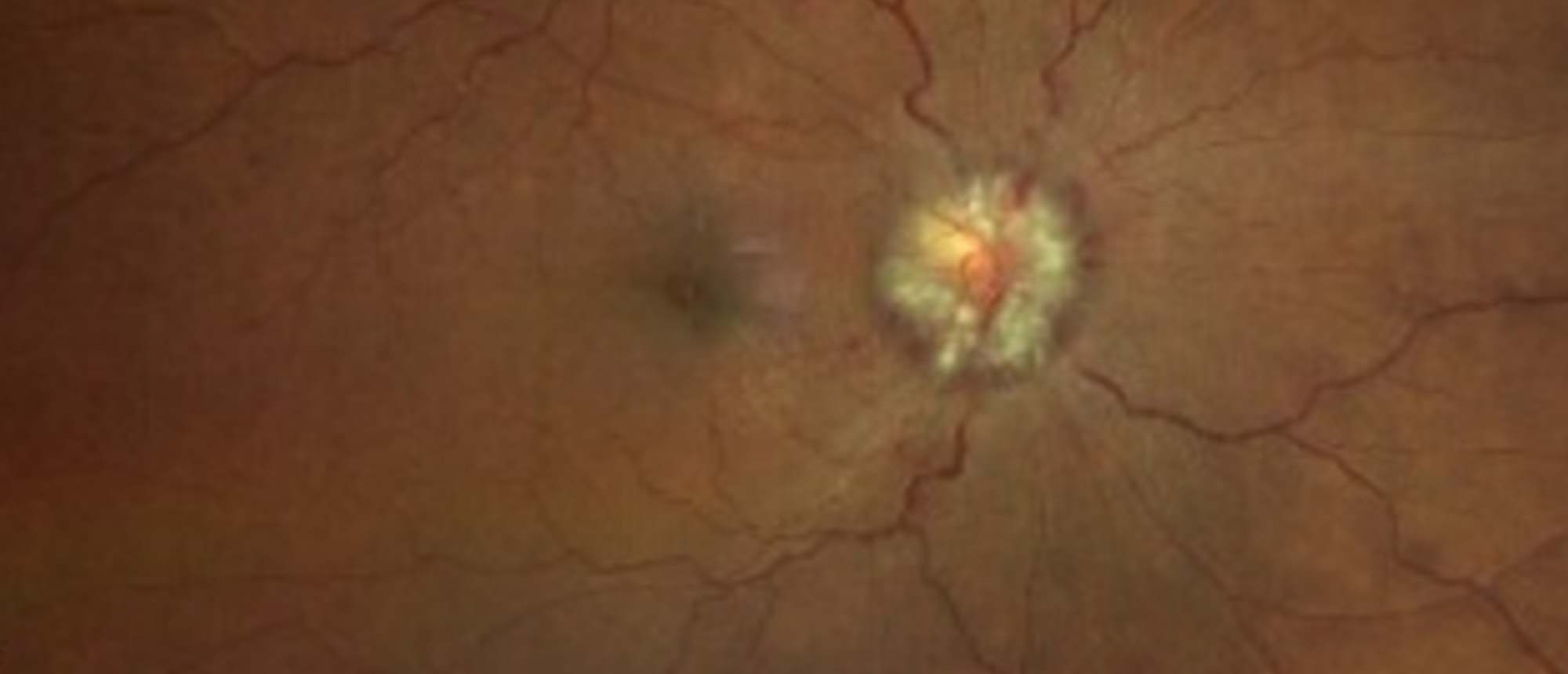
A patient presented with two weeks of vision loss alongside a year-long complaint of left-sided neck stiffness and headaches. Past medical history was remarkable for end-stage renal disease on peritoneal hemodialysis. Examination was notable for blood pressure of 170/104, VA 20/25 OD and 20/40 OS, bi-nasal inferior visual field defects, subtle abduction deficit OD, Grade IV-V optic disc edema with peripapillary heme and dot blot hemorrhages along the venous arcades, and absent venous pulsations. MRI brain, orbits, and MRV were remarkable for findings suggestive of increased intracranial pressure including increased optic nerve sheath diameter, flattened optic globes, flattened pituitary, and transverse venous sinus narrowing. The patient was intolerant to renally dosed acetazolamide and subsequently underwent transverse venous sinus stenting with near complete resolution of optic disc edema and vision loss. Perioperative monitoring utilizing virtual reality visual field demonstrated improvement following treatment interventions, with near-complete resolution observed 28-days post procedure. This case underscores the importance of timely diagnosis and treatment of Idiopathic Intracranial Hypertension (IIH), especially in high-risk populations such as those with end-stage renal disease. Non-surgical approaches are preferred initially, with surgical options reserved for cases of medical intolerance or rapid vision deterioration. This report also highlights the utility of virtual reality technology in bedside monitoring of visual field progression.
Presentation Date: 04/18/2024
Issue Date:04/26/2024
Please log in or click on ENROLL ME to access this course.