Pseudomonas Necrotizing Scleritis
Section outline
-
-
Description
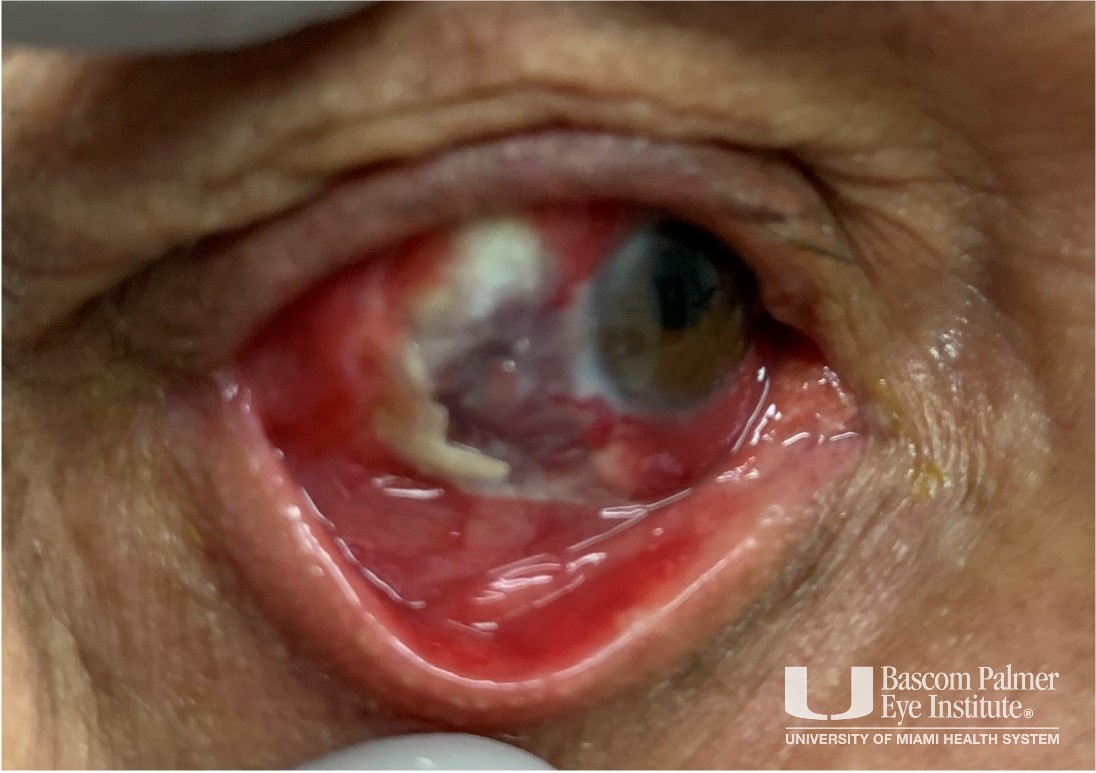
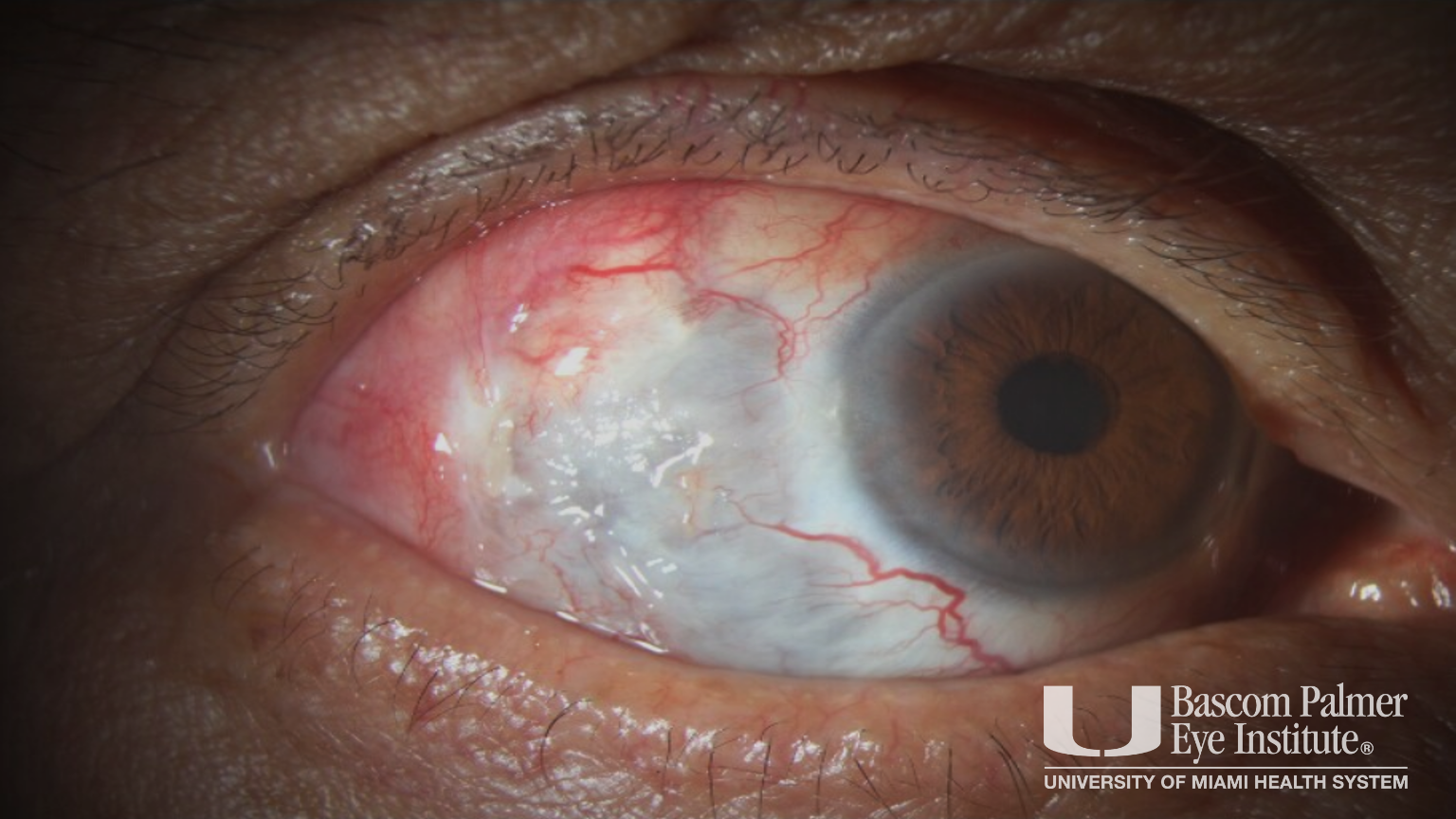
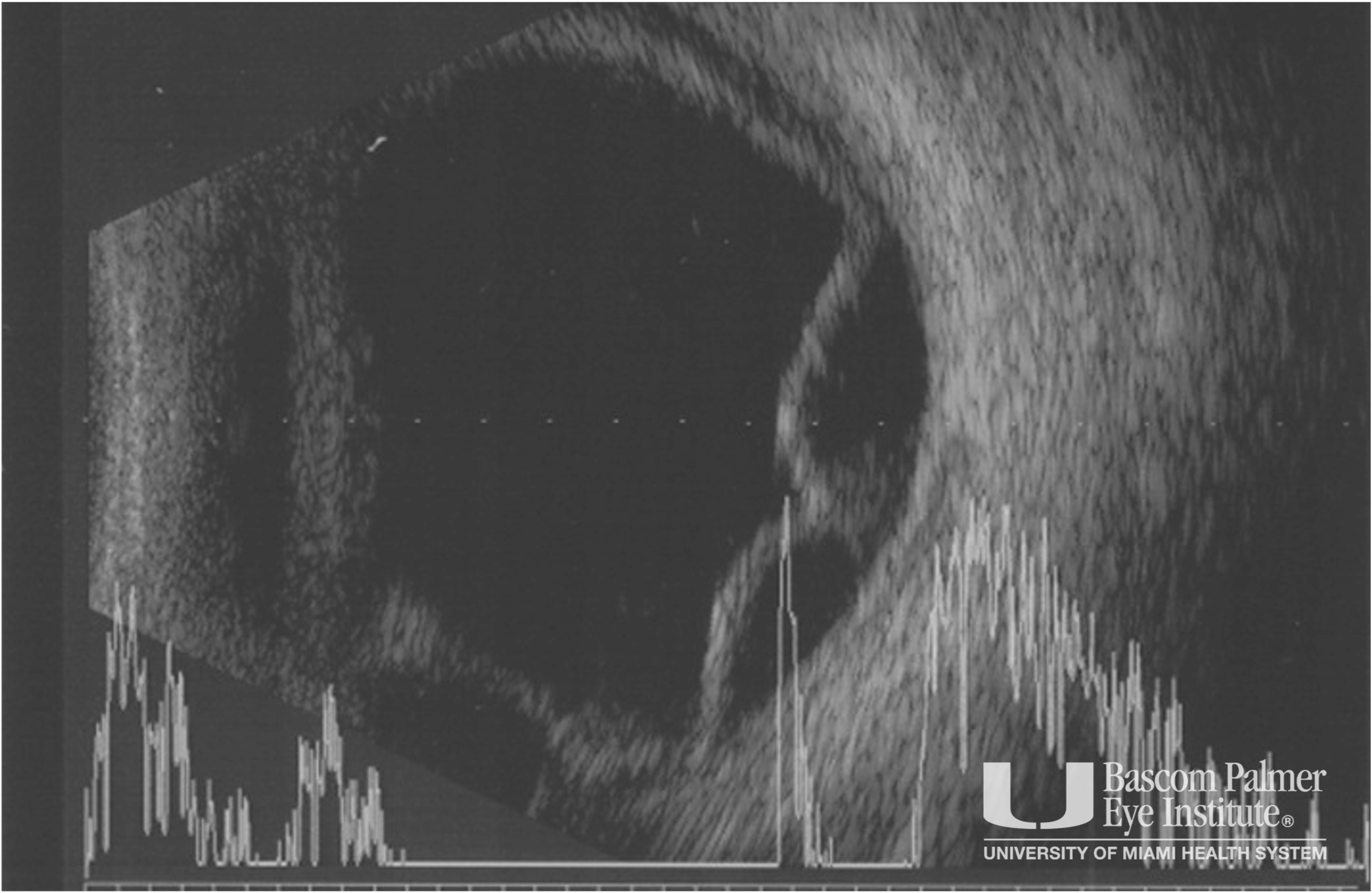
A patient with no past medical history and a past ocular history of five prior pterygium removal surgeries presented to the Bascom Palmer Emergency Room for pain and irritation in his right eye for 1 week. He endorsed working construction just prior to symptom onset, but denied any trauma to the eye, medication use, previous episodes, or history of autoimmune disease. On initial exam his visual acuity and intraocular pressure were 20/200 and 5 mm Hg in the right eye respectively compared to 20/20 and 16 mmHg in the left eye. Anterior segment exam of the right eye was remarkable for 3+ injection, nasal and inferotemporal areas of bare sclera with uveal show, and superotemporal and inferonasal areas concerning for abscess. 3+ flare was seen in the anterior chamber, and posterior synechiae and shallow choroidal detachments were identified, but no signs of perforation or corneal involvement were noted. B-scan imaging demonstrated choroidal detachments, but no foreign body, and CT scan of the orbits was also unremarkable. A culture of the sclera was taken, and infectious and inflammatory laboratories were sent for autoimmune and infectious causes of scleritis. He was started on topical and oral fluoroquinolones as well as high dose NSAIDs and oral doxycycline to prevent further thinning of the sclera. Culture results demonstrated Pseudomonas aeruginosa, and after 48 hrs of therapy, oral and topical steroids were begun. 72 hrs later, he underwent surgical debridement, subconjunctival antibiotics, and Rose Bengal photodynamic therapy (RB PDT). The patient stabilized, steroids and antibiotics were tapered over several weeks, and at 6 week follow up the visual acuity was 20/40, patient had fully epithelialized, and there were no remaining signs of infection.
Uploaded on: 07/31/2024